
Flickr user Bike SLO County (CC)
Thanks to a new community benefits category, hospitals can now fund projects that support healthy living, including bike lanes.
In Illinois, tax-exempt hospitals are required to spend 7.5 percent of operating revenues on community benefits. Historically, the vast majority—60 to 75 percent—of community benefit spending went toward charity or uncompensated care. However, the Affordable Care Act changed the game for nonprofit hospitals in many ways, including by revising tax exemption standards to include “community building,” defined by the Internal Revenue Service to include physical and environmental improvements, housing and economic development. This means that a hospital now can receive tax credits for investing in things like building a community park, improving infrastructure and building affordable housing.
What’s more, with more Americans insured because of the Affordable Care Act, many hospitals anticipate that the significant portion of their community benefits dollars previously spent on charity care will be freed up to be spent elsewhere—such as in our communities.
Enter community building benefits, which represent a tremendous opportunity for Chicago-area hospitals, planners and community leaders to develop new partnerships that vastly improve people’s lives and strengthen neighborhoods across the city and region. Consider the potential: Chicago’s hospitals spent a total of $3.6 billion in charitable community benefits in 2010, and hospitals across Illinois spent $5.5 billion.
Dougal Hewitt of Presence Health is excited about the promise of community benefits to support community development agendas of hospitals in the region. “This is an exciting time because previously there was greater competition amongst hospitals. This new community building category represents an opportunity for hospitals to collaborate for the benefit of our shared communities." What if, for example, the hospitals in the Illinois Medical District teamed up to make strategic investments in the developing communities that surround them? Or if other, larger healthcare networks collaborated to invest in pedestrian-friendly infrastructure? The Affordable Care Act also requires new reporting protocols for participating Illinois hospitals. This includes creating a community benefits spending plan every three years, referred to as a Community Health Needs Assessment, and delivering an interim annual report to document progress toward the goals outlined in the assessment. You can see an example of this assessment from Sinai Health System and an annual community benefits report from Rush Medical Center.
The Metropolitan Planning Council (MPC) has learned more about hospital community benefits through our Employer-Assisted Housing work, which has brought us to the table to discuss community development with local hospitals. Through these conversations, we’ve heard time and time again that hospitals are interested in improving community health beyond traditional healthcare. We’ve learned that community benefits historically have been spent in reaction to poor health rather than proactively to promote healthier lifestyles. In 2009, the Internal Revenue Service conducted a national survey of hospitals and found that hospitals interpret community benefits widely. MPC believes all of these factors point to an opportunity for community development practitioners and policy makers to forge relationships with the healthcare community.
“There’s been lots of collaboration between healthcare organizations but not so much between healthcare organizations and community organizations,” says Raul Raymundo, executive director of The Resurrection Project, a neighborhood organization that addresses issues related to education, housing, organizing and community development in several southwest communities.
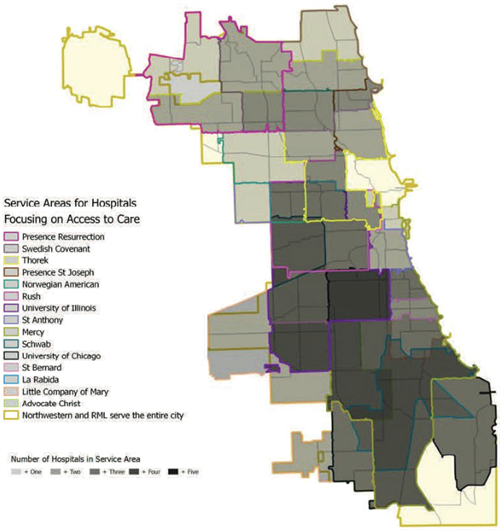
Chicago Department of Public Health
Chicago’s hospitals have overlapping service areas for certain areas of focus, like access to care or heart health. Overlapping service areas present a natural opportunity to collaborate more, especially when it comes to community development.
In the Chicago region, there are a number of healthcare collaborations, both vetted and emerging, city-focused and regional, working to improve the health of communities through hospital collaborations based on shared service areas and health priorities. MPC is currently participating in these collaborations to represent the community development component of the healthy communities that we all want for our region. A number of healthcare-oriented stakeholders have told us that they’d like to collaborate with nontraditional partners like MPC to improve community health. Some questions MPC would like to partner with the healthcare community to explore include:
- How can organizations like MPC work with hospital collaboratives to strengthen connections between community health and the built environment?
- Who else can we engage to help identify levers for change throughout the Chicago community?
- How can organizations like MPC partner with hospitals to leverage their community benefits for existing community priorities?
- How can we measure the impacts of this type of community health planning?
MPC will continue to explore this opportunity and hopes to be part of the discussion when Chicago’s regional stakeholders agree on what a healthy community is in the first place. Then we can move toward best practices such as in Rockford, Ill., where Swedish American Hospital committed $4.1 million to affordable housing development, or in Cleveland, where the Cleveland Clinic and University Hospitals of Cleveland bought $6.25 million naming rights for a bus rapid transit line, dubbed the HealthLine. The corridor has since attracted nearly $6 million in investment.
In May 2015, MPC hosted a discussion with external partners to hear from healthcare stakeholders and the planning community about this opportunity and how it fits with their organizational priorities. We’ve learned a lot through those gatherings: 1) hospitals are eager to collaborate with each other as well as with community development practitioners; 2) funding for Illinois healthcare institutions is extremely limited; 3) the Chicago region is eager to redefine health and healthy communities; and 4) many hospitals do not know about this new community building category. The Affordable Care Act’s impact on community benefits, coupled with these early lessons, represents an opportunity to bring Chicago-area hospitals together in a new way. Hospitals are true community anchors—providing care for the underinsured, responding to a community’s health needs, delivering critical research and acting as a major economic engine. MPC, known for connecting the dots, hopes to help these institutional anchors leverage their strategic investments for maximum benefits for their campuses and the communities that surround them.